Your Resources
Breast Cancer
Getting a mammogram is an important part of breast health for women, typically recommended for those aged 40 and older. Here are the general steps to get a mammogram:
- Consult Your Doctor: The first step is to consult your primary care physician or gynecologist. They can assess your risk factors and recommend when you should start getting mammograms and how often you should have them. In some cases, if you have a family history of breast cancer or other risk factors, you might need to start earlier.
- Schedule an Appointment: If your doctor recommends a mammogram, you’ll need to schedule an appointment at an imaging facility.
- Preparation: Before your mammogram, there are a few things to keep in mind:
- Avoid using deodorant, lotion, or powder on your chest and underarms on the day of the mammogram, as these products can interfere with the imaging.
- Wear a two-piece outfit, as you will need to undress from the waist up for the procedure.
- The Mammogram Procedure:
- You will be asked to stand in front of a specialized X-ray machine.
- A technologist will position your breast on a special platform and gently compress it with a plastic paddle to spread out the breast tissue. This is done to obtain clear images and might cause some discomfort, but it usually lasts only for a few seconds.
- The technologist will take X-ray images of your breast from different angles. You will typically have at least two images taken of each breast.
- Results and Follow-up: After your mammogram, a radiologist will review the images. If the results are normal, you’ll typically receive a letter in the mail and sent an annual reminder to complete another screening. If there are any concerning findings, your doctor will contact you to discuss further steps, which may include additional imaging or a biopsy. If a tumor is found to be cancerous, patients can be referred to Clearview Cancer Institute if medical oncology is part of the treatment plan.
Remember, regular mammograms are essential for early detection of breast cancer, which can significantly improve outcomes. Discuss your breast health and screening schedule with your healthcare provider to determine the best approach for your individual circumstances.
Breast Cancer
One in eight women will be diagnosed with breast cancer in their lifetime. It is the most commonly diagnosed cancer in women, making it the second leading cause of death. As with all types of cancer, breast cancer occurs when healthy cells become damaged and invade the surrounding tissue.
Breast Cancer Video FAQs
Patients with early stages of breast cancer often don’t have symptoms. This makes the need for yearly mammograms and regular self-examinations even more important in order to detect early stage breast cancer. The presence of these symptoms doesn’t necessarily mean you have breast cancer, but if you have one or more of the following symptoms, please consult your physician.
- Lump in the breast or underarm area
- Enlargement of pores around the breast or nipple area (often described as an orange peel’s texture)
- Dimpling on the breast
- Unexplained swelling or shrinkage of one of the breasts
- Inverted nipple
- Nipple discharge that is clear or bloody
Risk factors for breast cancer can be related to personal choices such as smoking, drinking, and diet. As you age, some of your risk factors can increase. Below is a list, although not inclusive, of risk factors for breast cancer.
- Age
- Family history
- Genetics
- Personal history of breast cancer
- Radiation to chest or face before the age of 30
- Race/ethnicity
- Being overweight
- Pregnancy or breastfeeding history (Breast feeding can lower the risk of breast cancer if a woman has breastfed longer than a year, and women who have never had children or had their first child after 30 have a higher risk than women who had their children before the age of 30.)
- Menstrual and menopause history (Women who started menstruating younger than age 12 have a higher risk, and the same is true for women who go through menopause when they are older than 55.)
- Using Hormone Replacement Therapy
- Drinking alcohol
- Having dense breasts
- Lack of exercise
- Smoking
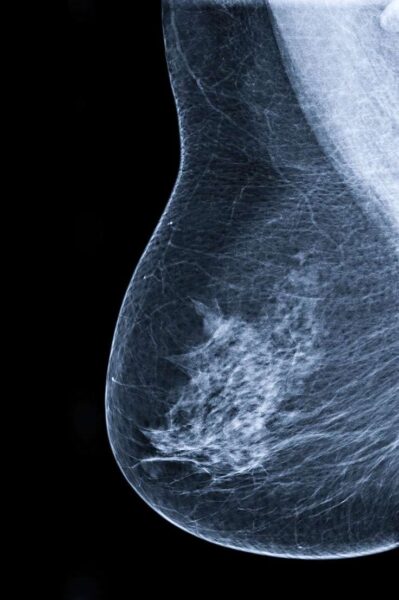
Early diagnosis of breast cancer plays a critical part in a patient’s treatment options and survival rates. Self breast exams and yearly mammograms are recommended screening tests to detect cancer in its early stages. Ultrasounds and MRIs are also used to support and categorize the diagnoses. Healthcare providers will commonly use ultrasound if the mammogram shows an unidentifiable mass. Sometimes the mass can be a fluid cyst, which can be mistaken for a solid cancer mass on a mammogram. A MRI, CT scan, and PET scan are all scans that may be used once a patient is diagnosed with cancer to help determine if the cancer has spread to other parts of the body. If your healthcare provider confirms a mass, but is not sure if it is cancerous, he may have to perform a surgical biopsy in order to look at the breast cells under a microscope and determine if they are cancer cells. Not all patients will need all of these tests. Each case if different and your physician will determine what tests are medically necessary.
Once the breast cancer has been diagnosed, your physician will discuss your treatment options. Treatment plans vary from patient to patient depending on a variety of factors. Two patients diagnosed with the same type of cancer may undergo different treatments depending on the stage of cancer, the location, or other underlying health issues. Clearview Cancer physicians treat each patient with individualized care making sure the treatment plan meets guidelines set by the National Comprehensive Care Network (NCCN) There are standard treatments which are current treatment options used by oncologists, and there are also clinical trials available which help advance the standard of care by offering patients regimens or new drugs currently not used as standard treatment. Breast cancer can be treated with one or more of the following treatment options:
Below are some of the more common types of breast cancer. This is not an inclusive list. For more information on breast cancer please visit americancancersociety.org
- Ductal Carcinoma in Situ (DCIS) is a very treatable early stage cancer where the damaged cells are in the lining of the breast milk duct but have not spread into the surrounding breast tissue.
- Invasive Ductal Carcinoma (IDC) originates in the milk ducts then spreads to the surrounding fatty tissue. Once these cancer cells break through the cell walls, they can remain near the milk duct or could enter the blood stream and metastasize, or spread, to other parts of the body. This is the most common type of breast cancer in women, and the type that commonly affects men. Invasive Ductal Carcinoma, or IDC, makes up 80% of all breast cancer diagnoses.
- Inflammatory Breast Cancer (IBC) is an aggressive cancer that spreads to the skin and lymph vessels of the breast. Because it doesn’t create lumps, early detection is more difficult. The skin surrounding the breast usually becomes red, swollen, and itchy similar to general inflammation symptoms. This is a rare type of breast cancer making up 1% of cancer diagnoses.
Stages
Determining the stage of breast cancer helps the physician decide the best course of treatment. Stages are determined based on the size of the tumor, the number of lymph nodes affected, and if the cancer has spread to other organs. The lower numbered stages represent the earlier detected breast cancers and the ones that are located closer to the point of origin in the milk ducts.
Stage 0
Ductal carcinoma in situ (DCIS), lobular carcinoma in situ (LCIS) and Paget disease of the nipple are all stage 0 breast cancers. In situ actually means, “in the original place.” Stage 0 breast cancers are highly treatable because they have not spread outside the milk duct walls. Self-examinations and yearly mammograms help detect stage 0 breast cancers before it spreads.
Stage I
Stage 1 cancer is still contained to the area where the cancer develops and it categorized by the size of the tumor. A stage 1 tumor is classified as 2 centimeters or smaller. Stage 1 breast cancers can also be classified by lymph nodes that have cancer evidence with clusters between .2mm and 2.0 mm
Stage II
Stage II breast cancer is very treatable and has not spread to other parts of the body. It is still contained in the breast or the lymph nodes near the breast. Stage II can be further broken down into Stage II A and Stage II B depending on the size of the tumor and if it is has spread into the lymph nodes. Most stage II tumors are classified as 2cm-5cm. However, stage IIA is classified as a tumor that can be less than 2cm, but is present in the nearby lymph nodes. For more detailed information regarding breast stage classification, please visit nationalbreastcancer.org
Stage III
Stage III breast cancer has spread outside the breast area and lymph nodes and has invaded the muscle but no other organs in the body. As in stage II, this stage is broken down into further categories of Stage IIIA, IIIB, and IIIC. Similar to the other stages, stage III classifications depend on the size of the tumor and how far the cancer cells have spread to the surrounding area and the number of lymph nodes affected. Tumors are larger than 5cm or have spread to 4-9 nearby lymph nodes to be classified as Stage III.
Stage IV
Stage IV breast cancer, also known as metastatic breast cancer, has spread to other areas and organs in the body (most often in the bones, lungs, liver, or brain). Most patients are diagnosed with metastatic cancer after they have completed treatment for earlier diagnosed breast cancer. Although the cancer has spread to other parts of the body, it is still classified and treated as breast cancer. While stage IV breast cancer is not curable, recent advances in maintenance drug therapy have extended the life of many stage IV cancer patients.
